11
11–14 APRIL, 2018, HELSINKI, FINLAND
CONCLUSIONS
Our findings provide evidence of a broad range of histologic alterations of the exstrophic bladder.
Persistent and partly progressing structural, inflammatory and proliferative changes are present in
a substantial proportion of patients despite succesful repair in early infancy. Importantly, intestinal
metaplasia, a potentially premalignant change, was not observed in any biopsy taken at primary
bladder closure, but only years thereafter during subsequent procedures. Since the natural history
of this lesion in the exstrophic bladder is unknown, these patients require lifelong surveillance.
13:33–13:36
S1-2 (PP)
PERSISTENT UROTHELIAL DIFFERENTIATION CHANGES
IN THE RECONSTRUCTED EXSTROPHIC BLADDER:
A PRIMARY STRUCTURAL DEFICIT?
Peter RUBENWOLF
1
, Fabian EDER
2
, Stefanie GOETZ
3
, Martin PROMM
4
and
Wolfgang H. ROESCH
4
1) University Hospital Frankfurt, Urology, Frankfurt, GERMANY - 2) University Hospital Regensburg, Pathology,
Regensburg, GERMANY - 3) University Hospital Regensburg, Urology, Regensburg, GERMANY - 4) University Hospital
Regensburg, Pediatric Urology, Regenburg, GERMANY
PURPOSE
To investigate whether the urothelial differentiation changes observed in the unclosed bladder
template persist after succesful delayed bladder closure in early infancy.
MATERIAL AND METHODS
Bladder biopsies from 34 children obtained during secondary reconstructive procedures were
examined by immunohistochemistry for expression cytokeratin 20, cytokeratin 13, claudin 4 and
uroplakin IIIa, all well characterised markers associated with the terminally differentiated urothelial
phenotype (group 1). Findings were compared with both bladder tissues harvested at the time of
primary delayed repair (group 2) and appropriate (non-exstrophy) controls (group 3).
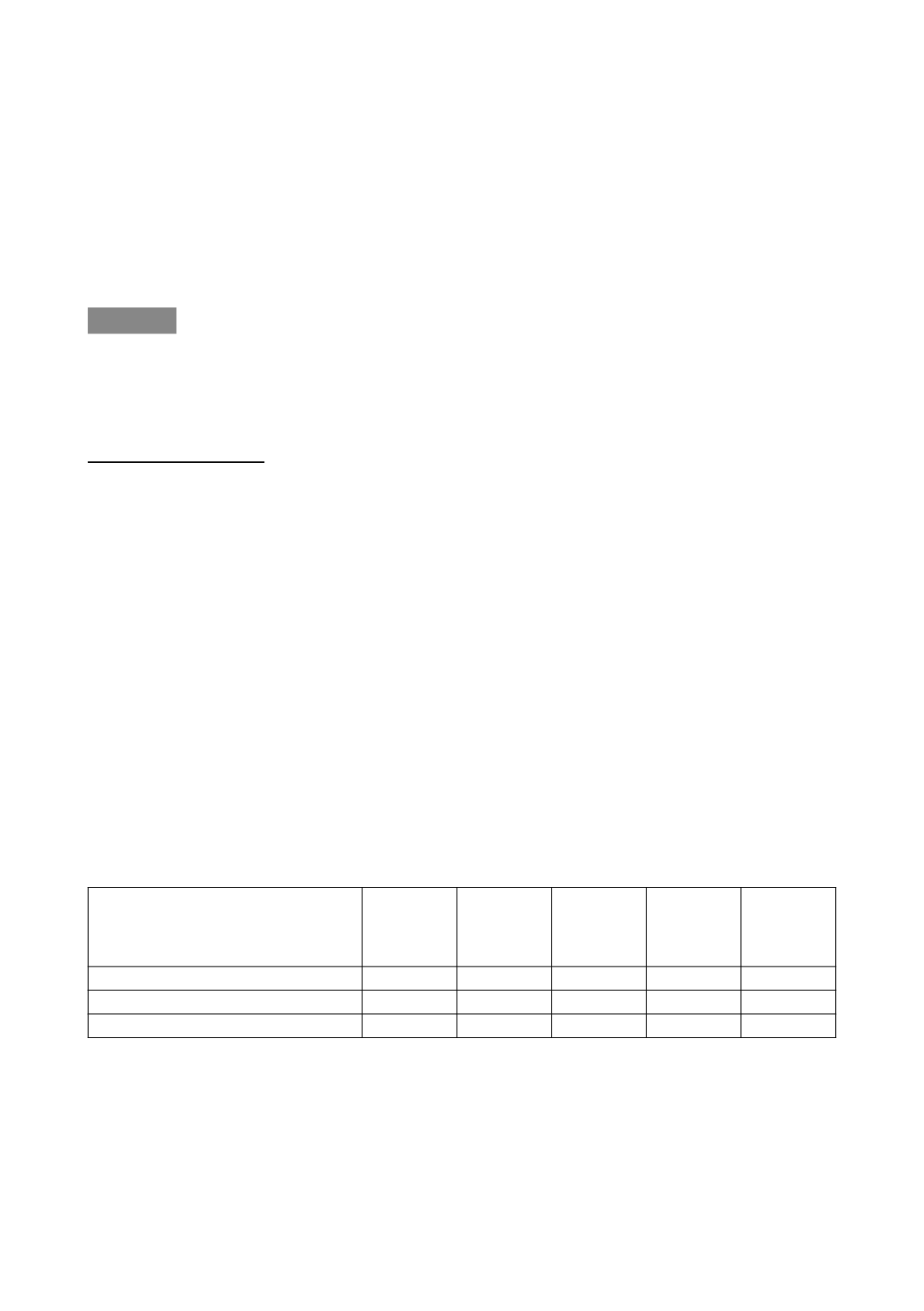
RESULTS
32 % of bladder specimen from children having previously undergone succesful primary bladder
closure displayed a regular urothelial morphology including umbrella cells and a fully differentiated
urothelial phenotype with regular expression of all 4 markers, as opposed to 4 % of bladders at the
time of primary reconstruction. Detailed results are presented in Table 1.
Group/Marker
(regular expression, %)
Cytokeratin
13
Cytokeratin
20
Claudin
4
Uroplakin
IIIa
Regular
expression
of all
4 markers
Group 1: reconstructed bladder (n=34)
47
35
71
35
32
Group 2: unclosed bladder (n=32)
34
4
48
4
4
Group 3: controls (no exstrophy; n=16)
93
97
89
95
89
CONCLUSIONS
Our finding provide prima facie evidence of persisting structural and phenotypic changes in two-
thirds of exstrophic bladders despite early bladder closure. In accordance with current genetic
findings, we hypothesize a primary genetically-determined structural and functional urothelial deficit
alongside a maturational delay and acquired secondary changes due to inflammatory and me-
chanical irritation of the unclosed urothelium. The translational value of our findings as regards the
developemental potential of the bladder needs to be established in future studies.